DEFINITON- A SHOCK STATE RESULTING FROM DECREASED INTRAVASCULAR VOLUME DUE TO FLUID LOSS
RISK FACTORS- TRAUMA, SURGERY, VOMITING, DIARRHEA, DIURESIS, DIABETES INSIPIDUS, HEMORRHAGE, BURNS, ASCITES, DEHYDRATION
PATHOPHYSIOLOGY :- DECREASED INTRAVASCULAR VOLUME---DECREASED VENOUS RETURN---DECREASED STROKE VOLUME---DECRESED CARDIAC OUTPUT---DECREASED TISSUE PERFUSION.
CLINICAL MANIFESTATIONS-DEHYDRATION, FATIGUE, HYPOTENSION,NAUSEA, PALLOR, OLIGURIA, TACHYCARDIA
RECOVERY POSITIONS- MODIFIED TREDLENBURG POSITION AKA PASSIVE LEG RAISING AS IT PROMOTES THE RETURN OF VENOUS BLOOD AND CAN BE USED AS A DYNAMIC ASSESSMENT OF PATIENT'S FLUID RESPONSIVENESS.
MEDICAL MANAGEMENT- IV FLUIDS- CRYSTALLOID SOLUTIONS SUCH AS LACTATED RINGER'S SOLUTION OR 0.9% NACL.
INSULIN IS GIVEN TO REVERSE THE CAUSE OF DEHYDRATION
ANTIDIARRHEAL AGENTS FOR DIARRHEA
ANTIEMETIC AGENTS FOR VOMITING
NURSING MANAGEMENT- 1.ADMINISTERING BLOOD AND FLUIDS SAFELY.
2.IMPLEMENTING OTHER MEASURES-OXYGEN ADMINISTRATION, PROVIDING COMFORT, MONITORING VITAL SIGNS, MAINTAINING I&O CHART, MONITORING ABG LEVELS, SERUM LACTATE LEVELS, HAEMOGLOBIN
DEFINITION : A SUBSET OF SEPSIS IN WHICH UNDERLYNG CIRCULATORY AND CELLULAR METABOLISM ABNORMALITIES ARE PROOUND ENOUGH TO SUBSTATIALLY INCREASE MORTALITY
CLINICAL MANIFESTATIONS:
-Cool, pale arms and legs.
-High or very low temperature, chills.
-Lightheadedness.
-Little or no urine.
-Low blood pressure, especially when standing.
-Palpitations.
-Rapid heart rate.
-Restlessness, agitation, lethargy, or confusion.
RISK FACTORS:-
Extremes of age (70 years)
-Primary diseases (eg, liver cirrhosis, alcoholism, diabetes mellitus)
-Immunosuppression (eg, from neutropenia, immunosuppressive therapy [eg, in organ and bone marrow transplant recipients], corticosteroid therapy)
-Major surgery, trauma, burns
-Invasive procedures (eg, placement of catheters, intravascular devices, prosthetic devices)
-Previous antibiotic treatment
-Prolonged hospitalization
-Underlying genetic susceptibility
-Other factors (eg, childbirth, abortion, and malnutrition)
MEDICAL MANAGEMENT: If the infecting organism is unknown, broad-spectrum antibiotic agents are started until culture and sensitivity reports are received
A third generation cephalosporin plus an aminoglycoside may be prescribed initially. This combination works against most gram-negative and some gram-positive organisms.
NURSING MANAGEMENT:- Infection control. All invasive procedures must be carried out with aseptic technique after careful hand hygiene.
-Monitor blood levels. The nurse must monitor antibiotic toxicity, BUN, creatinine, WBC, hemoglobin, hematocrit, platelet levels, and coagulation studies.
-Assess physiologic status. The nurse should assess the patient’s hemodynamic status, fluid intake and output, and nutritional status
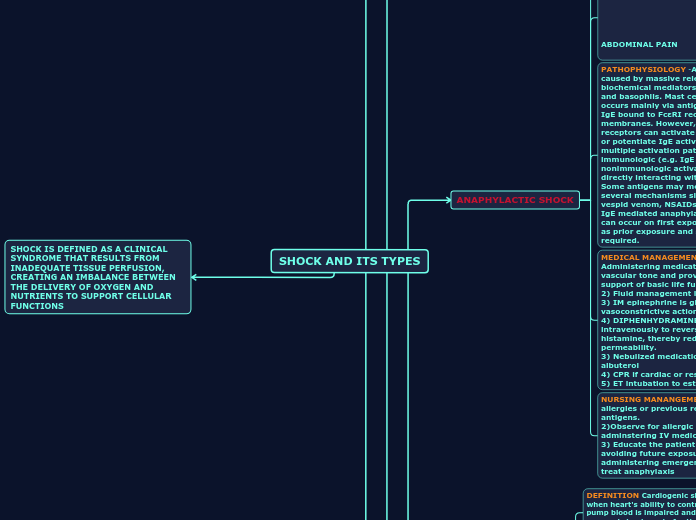
DEFINITION: DISTRIBUTIVE SHOCK STATE RESULTING FROM A SEVERE ALLERGIC EACTION PRODUCING AN ACUTE SYSTEMIC VASODILATION AND RELATIVE HYPOVOLEMIA
CLINICAL MAIFESTATIONS: 1.HYPOTENSION
2.NAUSEA
3.TACHYCARDIA
4.DYSPNEA
5.DIARRHOEA
6.ACUTE ABDOMINAL PAIN
7.PRURITIS
PATHOPHYSIOLOGY -Anaphylaxis is caused by massive release of biochemical mediators from mast cell and basophils. Mast cells activation occurs mainly via antigen crosslinking of IgE bound to FcεRI receptors on cell membranes. However, other membrane receptors can activate mast cells as well or potentiate IgE activation . The multiple activation pathways allow for immunologic (e.g. IgE mediated) and/or nonimmunologic activation (e.g. drug directly interacting with receptors). Some antigens may mediate effects via several mechanisms simultaneously (e.g. vespid venom, NSAIDs, opiates). In non-IgE mediated anaphylaxis, symptoms can occur on first exposure to an antigen as prior exposure and sensitization is not required.
MEDICAL MANAGEMENT:1) Administering medications that restore vascular tone and providing emergency support of basic life functions.
2) Fluid management is critical
3) IM epinephrine is given for its vasoconstrictive action
4) DIPHENHYDRAMINE is given intravenously to reverse action of histamine, thereby reducing capillary permeability.
3) Nebulized medications such as albuterol
4) CPR if cardiac or respiratory arrest
5) ET intubation to establish airway
NURSING MANANGEMENT: 1) Assess for allergies or previous reactions to antigens.
2)Observe for allergic reactions while adminstering IV medications.
3) Educate the patient and family about avoiding future exposure to antigens and administering emergency medications to treat anaphylaxis
DEFINITION Cardiogenic shock occurs when heart's ability to contract and to pump blood is impaired and the supply of oxygen is inadequate for the heart and tissues.
PATHOGENESIS: decreased cardiac contractility----decreased stroke volume and cardiac output ------causes pulmonary congestion, decreased systemic tissue perfusion, decreased coronary artery perfusion.
CLINICAL MANIFESTATIONS:- angina pain, dysrhythmias, fatigue, feelings of doom, signs of hemodynamic instability.
RISK FACTORS: Older age.
Heart failure.
A prior heart attack – this risk is higher among women.
Coronary heart disease.
High blood pressure.
Diabetes
MEDICAL MANAGEMENT:A) oxygenation
B) pain control
C)hemodynamic monitoring
D) fluid therapy
E) pharmacologic therapy- dobutamine, nitroglycericine, dopamine
F) mechanical assistive devices
NURSING MANAGEMENT: 1) preventing Cardiogenic shock
2) Identifying at risk patients early
3)promoting adequate oxygenation of the heart muscle, and decreasing cardiac workload can prevent Cardiogenic shock.
4) The major role of nurses monitoring the patients he more dynamic and cardiac status to see that arterial lines and ECG monitoring equipment must be well maintained and functioning properly.
Changes in hemodynamic cardiac and pulmonary status and laboratory values are documented, breath sounds ,changes in cardiac rhythm and other abnormal physical assessment findings are reported immediately
5) administering medications and iv fluids
6) enhancing safety and comfort
DEFINITION: SHOCK STATE RESULTING FROM LOSS OF SYMPATHETIC TONE CAUSING RELATIVE HYPOVOLEMIA
CLINICAL MANIFESTATIONS: HYPOTENSION, HYPOTHERMIA, BRADYCARDIA
RISK FACTORS: SPINAL CORD INJURY, SPINAL ANESTHESIA, DEPRESSANT ACTION OF MEDICATION, HYPOGLYCEMIA
MEDICAL MANAGEMENT: PREVENT SHOCK, MAINTAIN AIRWAY PATENCY, AVOID COMPLICATIONS SUCH AS STOOL OR URINE RETENTION, REPIRATORY AND CARDIOVASCULAR DIFFICULTY, AND FORMATION OF DEEP VEIN CLOTS
NURSING MANAGEMENT: MONITOR VITAL SIGNS, OXYGENATION, ASSESS HEMODYNAMIC AND NEUROLOGIC PARAMETERS INCLUDIN MOTOR SENSTATION AND REFLEXES.
DEFINITION: SHOCK STATE RESULTING FROM DISPLACEMENT OF INTRAVASCULAR VOLUME CREATING A RELATIVE HYPOVOLEMIA AND INADEQUATE ELIVERY OF OXYGEN TO THE CELLS
CLINICAL MANIFESTATIONS: tachypnea, tachycardia, low to normal blood pressure, decreased urine output, and decreased level of consciousness.
PATHOPHYSIOLOGY:- PRECIPITATING EVENT--VASODILATION--ACTIVATION OF INFLAMMATORY RESPONSE--MALDISTRIBUTION OF INTRAVASCULAR VOLUME--DECREASED VENOUS RETURN--DECREASED CARDIAC OUTPUT--DECREASED TISSUE PERFUSION.
RISK FACTORS:SIRS due to noninfectious conditions such as pancreatitis, burns, or trauma.
TSS.
Anaphylaxis.
Adrenal insufficiency.
Reactions to drugs or toxins.
Heavy metal poisoning.
Hepatic insufficiency.
Neurogenic shock.
MEDICAL MANAGEMENT: The main goals of treatment in distributive shock are to reverse the underlying cause and achieve hemodynamic stabilization. Immediate treatment involves fluid resuscitation and the use of vasoactive drugs, both vasopressors and inotropes.These medications are used to treat low blood pressure. They include dopamine, epinephrine (Adrenaline, Auvi-Q), norepinephrine (Levophed)
NURSING MANAGEMENT: The key is to maintain a perfusion pressure of at least 65 mmHg.
- Fluids are usually the first choice treatment followed by the use of vasopressors.
- The primary cause of distributive shock must be identified and treated if the outcome is to be improved.
- To monitor the patient for urine output, hemodynamic stability, oxygenation, ventilation and provide prophylaxis against DVT and stress ulcers.