Boehning, A. P., & Punsalan, L. D. (2023, March 1). Advanced practice registered nurse roles.StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK589698/
Baker, K., & Williams, T. E. (2016). Overview and summary: Elimination of barriers to RN scope of practice: Opportunities and challenges. Online Journal of Issues in Nursing, 21(3). https://doi.org/10.3912/OJIN.Vol21No03ManOS
Feringa, M. M., De Swardt, H. C., & Havenga, Y. (2018). Registered nurses’ knowledge, attitude, practice and regulation regarding their scope of practice: A literature review. International Journal of Africa Nursing Sciences, 9, 1–8. https://doi.org/10.1016/j.ijans.2018.04.001
Kleinpell, R., Myers, C. R., Likes, W., & Schorn, M. N. (2022). Breaking down institutional barriers to advanced practice registered nurse practice. Nursing Administration Quarterly, 46(2), 137–143. https://doi.org/10.1097/NAQ.0000000000000518
Wheeler, K. J., Miller, M., Pulcini, J., Gray, D., Ladd, E., & Rayens, M. K. (2022). Advanced practice nursing roles, regulation, education, and practice: A global study. Annals of Global Health, 88(1), 42. https://doi.org/10.5334/aogh.3698
Kleinpell, R., Myers, C. R., & Schorn, M. N. (2023). Addressing barriers to APRN practice: Policy and regulatory implications during COVID-19. Journal of Nursing Regulation, 14(1), 13–20. https://doi.org/10.1016/S2155-8256(23)00064-9
Peterson, M. E. (2017). Barriers to practice and the impact on health care: A nurse practitioner focus. Journal of the Advanced Practitioner in Oncology, 8(1), 74–81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5995533/
Barton, M. J., Hannum, B. C., Lindsey, M., & Towle, T. (2020). The path toward full practice authority: One state’s strategy. The Journal for Nurse Practitioners, 16(10), 760–763. https://www.npjournal.org/article/S1555-4155(20)30513-4/pdf
Mark, D. (2023). Advocating for policy change: The role of advanced practice nurses in healthcare reform. Journal of Advanced Practices in Nursing, 8(4). https://www.hilarispublisher.com/open-access/advocating-for-policy-change-the-role-of-advanced-practice-nurses-in-healthcare-reform.pdf
Morris, G. (2024, February 22). Why policy engagement is the next big nursing trend. NurseJournal. https://nursejournal.org/articles/the-role-of-nurses-in-policy-engagement/
Zalon, M. L., Ludwick, R., & Patton, R. M. (2024). Strengthening nurses' influence in health policy. AJN, American Journal of Nursing, 124(9), 28–36. https://doi.org/10.1097/01.NAJ.0001028316.80475.bf
Tapp, J., Ketel, C., Vick, R., Zsamboky, M., Pfieffer, M. L., Gardner, V., Cole, S., & Pitts, C. (2025). Closing the provider gap in rural and underserved communities: Preparing family nurse practitioner students for entry-to-practice. Nurse Educator, 50(1), E1 E6. https://doi.org/10.1097/NNE.0000000000001723
Taylor, K. (2023). Bridging the gap to health care access: The role of the nurse practitioner. International Archives of Public Health and Community Medicine, 7(91). https://doi.org/10.23937/2643-4512/1710091
Yates, M. C., Auerbach, D. I., Staiger, D. O., & Buerhaus, P. I. (2022). Characteristics of rural registered nurses and the implications for workforce policy. The Journal of Rural Health, 39(1), 93–100. https://doi.org/10.1111/jrh.12707
National Academies of Sciences, Engineering, and Medicine. (2016). Assessing progress on the Institute of Medicine report The Future of Nursing. The National Academies Press. https://doi.org/10.17226/21838
Hain, D., & Fleck, L. M. (2014). Barriers to NP practice that impact healthcare redesign. Online Journal of Issues in Nursing, 19(2), 2. https://doi.org/10.3912/OJIN.Vol19No02Man02
Chiu, P., Cummings, G. G., Thorne, S., & Schick-Makaroff, K. (2021). Policy advocacy and nursing organizations: A scoping review. Policy, Politics & Nursing Practice, 22(4), 271–291. https://doi.org/10.1177/15271544211050611
Rash, M. (2024, May 13). NC Institute of Medicine releases recommendations for strengthening the state’s nursing workforce. EdNC. https://www.ednc.org/05-13-2024-nciom-releases-recommendations-for-strengthening-ncs-nursing-workforce/
Sutor, A., & Painter, J. (2020). Nurse residency programs: Providing organizational value. Delaware Journal of Public Health, 6(1), 58–61. https://doi.org/10.32481/djph.2020.04.013
Ferguson, S. L. (1998). Impacting public policy: Fellowships; internships foster nursing leaders. Health Care Advocate, 2(2), 24–26. https://doi.org/10.1111/j.1552-6356.1998.tb01006.x
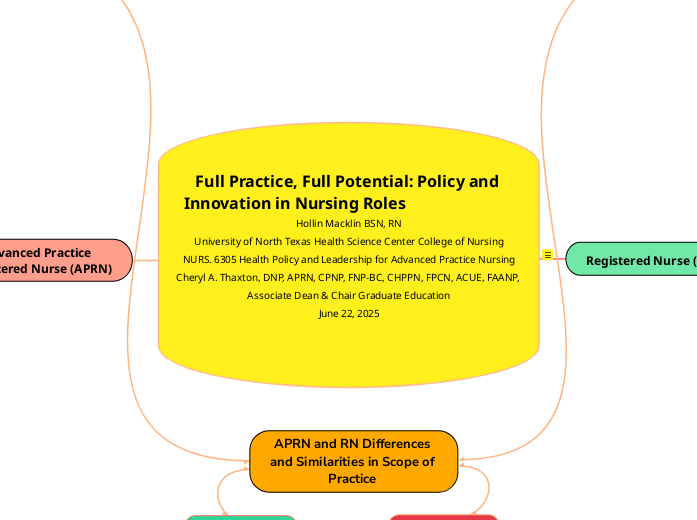
Similarities:
Differences:
APRNs possess deeper theoretical knowledge, advanced clinical skills, and are perceived as more autonomous
APRNs have independent diagnostic and prescribing authority (APRN)
RN's typically do not operate independently
Both play major roles in Patient advocacy
, Health promotion, and education
Both roles work collaboratively with physicians and other care team members.
Equally accountable and responsible for patient care within their legal and institutional frameworks.
Both emphasize holistic, dignified, patient-centered care, advocacy, and follow similar laws, protocols, and regulations.
APRN and RN Differences and Similarities in Scope of Practice
Leadership in care management (APRN)
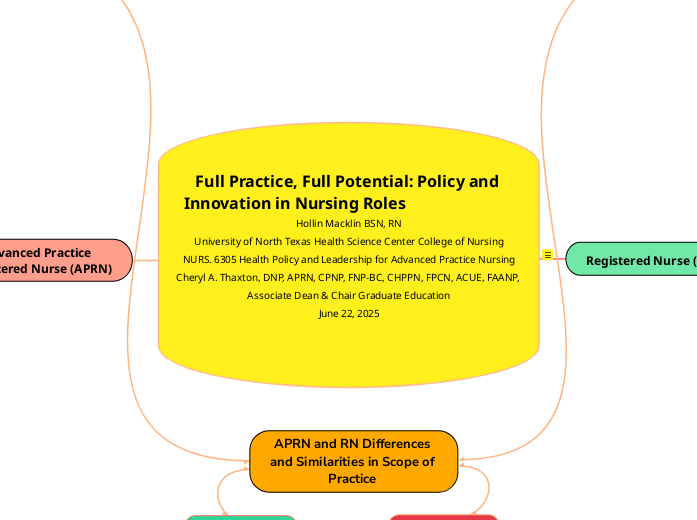
Full Practice, Full Potential: Policy and Innovation in Nursing Roles Hollin Macklin BSN, RN
University of North Texas Health Science Center College of Nursing
NURS. 6305 Health Policy and Leadership for Advanced Practice Nursing
Cheryl A. Thaxton, DNP, APRN, CPNP, FNP-BC, CHPPN, FPCN, ACUE, FAANP, Associate Dean & Chair Graduate Education
June 22, 2025
Full Practice, Full Potential: Policy and Innovation in Nursing Roles
Central Topic:
Full Practice, Full Potential: Policy and Innovation in Nursing Roles
Subtopic 1: Registered Nurse (RN)
Sub-subtopic: RN Scope of Practice
Provides direct care under supervision of APRNs or physicians
Administers medications, monitors vital signs, and offers emotional and educational support
Cannot diagnose conditions or prescribe medications
Education: Associate Degree in Nursing (ADN) or Bachelor of Science in Nursing (BSN)
Integral in patient care coordination and advocacy
(Jersey College, 2025)
Sub-subtopic: Differences and Similarities to APRNs
RNs cannot diagnose or prescribe, unlike APRNs
APRNs have advanced degrees and greater clinical autonomy
Both RNs and APRNs serve as patient advocates and educators
Sub-subtopic: Key Barriers to Full Practice (RN)
Legal: Narrowly defined scope-of-practice laws
Regulatory: Lack of national licensure standardization
Institutional: Limited decision-making roles within clinical settings
(Feringa et al., 2018; Kleinpell et al., 2022)
Sub-subtopic: Strategies to Engage Stakeholders (RN)
Share outcome data showcasing RN impact
Develop partnerships with hospital leadership
Advocate via state nursing associations for SOP updates
(Zalon et al., 2024)
Sub-subtopic: Addressing Rural & Underserved Needs (RN)
Support nurse-led clinics and mobile health units
Train RNs from rural communities through targeted scholarships
Emphasize care coordination and chronic disease management
(Yates et al., 2022)
Sub-subtopic: Policy/Organizational Changes & Advocacy (RN)
Promote uniform licensure and privilege expansion
Campaigns led by ANA and local coalitions
Develop rural RN advocacy fellowships and legislative internships
Use data dashboards to highlight RN shortages and outcomes
Subtopic 2: Advanced Practice Registered Nurse (APRN)
Sub-subtopic: APRN Scope of Practice
Includes NP, CNM, CRNA, CNS roles
Can diagnose, prescribe, and independently manage care
Authorized for independent practice in 26 states
Requires a Master's or Doctoral degree
(Boehning & Punsalan, 2023)
Sub-subtopic: Key Barriers to Full Practice (APRN)
Legal: Restrictive SOP laws, required physician oversight
Regulatory: Lack of consistent credentialing frameworks
Institutional: Denied privileges in hospital systems or limited EHR access
(Hain & Fleck, 2014; Peterson, 2017)
Sub-subtopic: Strategies to Engage Stakeholders (APRN)
Leverage data showing APRN cost-effectiveness and quality outcomes
Engage through national policy briefings and interprofessional forums
Work with Future of Nursing Campaign and AANP
(Mark, 2023)
Sub-subtopic: Addressing Rural & Underserved Needs (APRN)
Expand telehealth and remote prescribing services
Launch APRN residency programs in rural FQHCs
Build community trust through culturally responsive care
(Tapp et al., 2025)
Sub-subtopic: Policy/Organizational Changes & Advocacy (APRN)
Advocate for APRN Consensus Model adoption
Partner with FTC to counter anticompetitive supervision mandates
Create storytelling-based campaigns showing APRN patient impact
Expand CMS reimbursement rules and hospital privileging reforms
(National Academies of Sciences, Engineering, and Medicine, 2016; FTC, 2014)
Advanced Practice Registered Nurse (APRN)
Policy/Organizational Changes & Advocacy (APRN) (National Academies, 2016; Kleinpell et al., 2023; Mark, 2023)
Empower APRN students through policy fellowships and media training
Expand CMS reimbursement rules and hospital privileging reforms
Use FTC and CMS data to advocate for removal of anticompetitive policies
Promote standardization via the APRN Consensus Model
Push for APRN Compact legislation for multi-state practice
Addressing Rural & Underserved Needs (APRN) (Tapp et al., 2025; Taylor, 2023)
Build community trust and retention through culturally responsive care
Launch APRN residency programs in rural FQHCs
Expand telehealth and remote prescribing services
Strategies to Engage Stakeholders (APRN) (Mark, 2023; Zalon et al., 2024)
Leverage AANP, ANA, and interdisciplinary coalitions
Engage through national policy briefings and interprofessional forums
Leverage data showing APRN cost-effectiveness and quality outcomes
Key Barriers to Full Practice (APRN)
Institutional: Restrictions on prescriptive authority, hospital admitting, and billing (Kleinpell et al., 2022; Barton et al., 2021)
Regulatory: Inconsistent certification, privileging, and transition-to-practice mandates (Feringa et al., 2018; Kleinpell et al., 2023)
Legal: SOP laws require physician collaboration in many states (Peterson, 2017; Hain & Fleck, 2014)
APRN Scope of Practice (Boehning & Punsalan, 2023)
Emphasizes evidence-based practice, leadership, health policy, and systems-level care
Requires a Master's or Doctoral degree
Authorized for independent practice in 26 states
Can diagnose, prescribe, and can independently manage care
Includes 4 Main Roles
Clinical Nurse Specialist (CNS)
Certified Registered Nurse Anesthetist (CRNA)
Certified Nurse-Midwife (CNM)
Nurse Practitioner (NP)
Registered Nurse (RN)
Policy/Organizational Changes & Advocacy (RN) (Chiu, Cummings, Thorne, & Schick-Makaroff, 2021; Rash, 2024; Sutor & Painter, 2020; Ferguson, 1998)
Expand BSN-preparation mandates and create RN residency programs
Launch storytelling campaigns through the Campaign for Action
Use data dashboards to highlight RN shortages and outcomes
Develop rural RN advocacy fellowships and legislative internships
Addressing Rural & Underserved Needs (RN) (Yates et al., 2022)
Support legislation recognizing RN clinical decision-making authority
Emphasize care coordination and chronic disease management
Train RNs from rural communities through targeted pipeline programs and scholarships
Empower nurse-led clinics and home visit models
Strategies to Engage Stakeholders (RN) (Zalon et al., 2024; Morris, 2024)
Use ANA’s Healthy Nurse Healthy Nation and Future of Nursing framework as leverage
Collaborate with hospital boards and quality councils
Present patient safety and quality metrics tied to RN-led interventions
Key Barriers to Full Practice (RN)
Institutional: Hospital policies limit RN protocol use and nurse-initiated care pathways (Kleinpell et al., 2022)
Regulatory: Inconsistent national licensure and lack of privileging policies (Feringa et al., 2018)
Legal: Scope-of-practice statutes limit autonomous roles (Baker & Williams, 2016)
RN Scope of Practice (Jersey College, 2025)
Integral in patient care coordination and advocacy
Requires: ADN or BSN
Cannot diagnose conditions or prescribe medications
Administers medications, monitors vital signs, and offers emotional and educational support
Provides direct care under supervision of APRNs or physicians