przez Danica Sanchez 1 rok temu
162
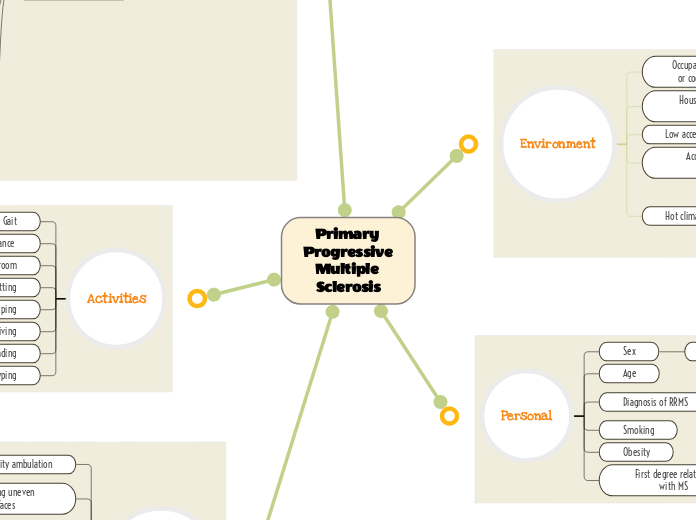
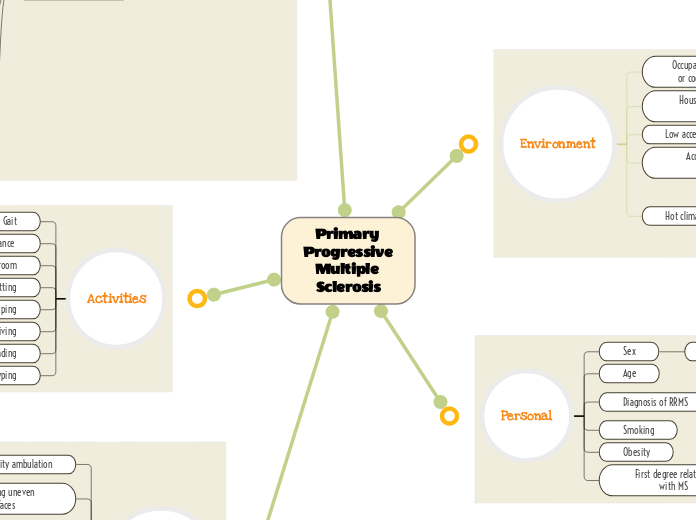
Primary Progressive Multiple Sclerosis
przez Danica Sanchez 1 rok temu
162
Więcej takich
Guides POC to see extent of patient's weakness and to set intensity and modality of exercises given to pt
If the patient has a steppage gait due to foot drop, it would interfere with learning a new gait pattern that involves active use of the weak dorsiflexors
Making sure that the exercises that work the weaker muscles aren't too easy, and the patient feels challenged
If you don't target the weak dorsiflexion and hemiparesis, it will atrophy and get worse
Focusing on the weaker side of the body to improve its functions and recruitment
Efficacy of muscle contractions depend on this tract running through myelinated structures
Left arm hemiparesis
Foot drop
The training for dynamic balance should be blocked at first to improve her foundations of gait then be transferred to random to mimic a variety of surfaces she'll encounter in her environment
Determine what other parts of ambulatory activities the patient struggles with
Walking on level surface, changing gait speed, gait with horizontal and vertical head turns, gait with pivot turn, stepping over and around obstacles, walking up stairs
When patient improves dynamic balances over firm surfaces, we can transfer her over to compliant surface ambulation to help her deficit of ambulating over uneven surfaces outside of the clinic.
Emphasizing that if ambulation improves, patient will be able to do more independent tasks by herself such as grocery shopping and socializing with friends.
Measures hand dexterity; patient is timed and places the pegs in the holes as quickly as possible
Taking her age into account, though it is possible to make neuroplastic changes, it may take a while compared to a younger patient
Professionally educate the patient about a realistic timeline and what it would take for how long it would take to achieve her goal to type with two hands
Including exercises that target the specific fine motor deficits that she struggles with
Incorporating a good HEP to get extra repetitions in for her fine motor exercises especially because this is one of her main goals
At first we should break the dual tasking into parts, and then slowly integrate practicing both at the same time as a whole
Measures cognitive dual tasking; patient starts from sit, stands up, and walks 3 meters and back while doing a cognitive task (ex: counting backwards from 100 by 5s), then sits down as quickly as possible
Since the patient has trouble with doing both cognitive and motor tasks at the same time, they compensate by stopping one task to complete the other. Slowly integrate dual tasking into treatment parameters.
Stimulating this area during PT will prevent further decline in cognitive processing
It is important to note that she has been diagnosed with MS since 2010, so her brain will not make neuroplastic changes as easily as someone with a fresher brain injury
However this means that we need to start working on more neuroplastic changes ASAP because the sooner the better
Make exercises functional to reinforce the Papez circuit and help with processing
To figure out if the lack of balance is due to lesions to corticospinal tract or DCML
Providing the pt a HEP that allows her to safely practice static balance in order to get the proper amount of repetitions in to make neuroplastic changes
Distributed practice conditions should be utilized to ensure the patient's fatigue doesn't interfere with her treatment
To determine extent of fatigue and to set parameters of how intense exercises should be in regular POC and what the progression would look like; Follow up with questions about what type of fatigue the patient is feeling
Working on endurance and managing fatigue symptoms will transfer over to improving her ability to attend longer social events
Including exercises and patient education in the pt's program that specifically addresses and helps improve fatigue
The exercises should adequately challenge the patient, yet not overfatigue them
Saltatory conduction makes neurons fire faster, without this myelination from the upper motor neurons, not as many action potentials will get through to the lower motor neurons, decreasing endurance of those structures.
Showering
Shower has 2 grab bars
Dressing
Can only wear sports bras and shirts that can be pulled on
Cleaning
Struggles with hanging clothes
Cooking
Has special kitchen appliances that help with this
Unable to have stairs in the home
Can't go to the store by herself
Spinal cord white matter
Corticospinal tract
Hemiparesis
Foot drop
AFO
Fasciculus cuneatus/gracilis
DCML
Loss of sensation (fine touch, vibration)
Problems with proprioception and balance
Thalamic nuclei
Ventrolateral
Problems with active movements of the contralateral side
Pons
Cranial nerve nuclei 5-8
CN 7: facial nerve
Taste loss
Micturition/storage centers
Bowel, bladder issues
Optic nerve
Vision problems
Limbic system + frontal cortex
Olfaction problems
Motor deficits
Gross motor
Fine motor
Trouble with processing, learning, and memory
Demyelination in the CNS
Slower action potentials
Weakness
Fatigue
Initially diagnosed with RRMS 2010 befrre PPMS
Female
Family lives in Florida, doesn't want to move up North, so just stays indoors during hot weather
Is unable to have stairs in the home