jonka Ashley Mann 3 vuotta sitten
213
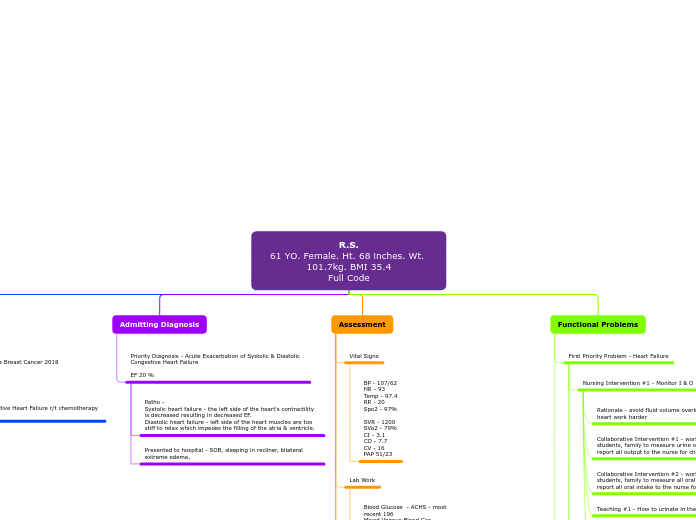
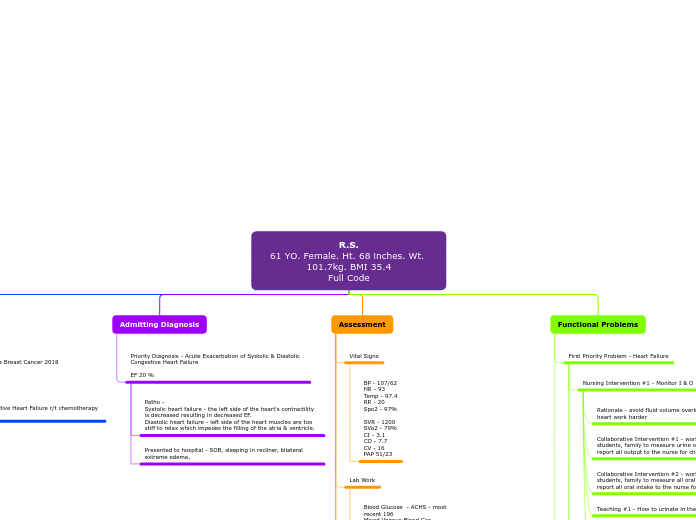
R.S. 61 YO. Female. Ht. 68 inches. Wt. 101.7kg. BMI 35.4 Full Code
jonka Ashley Mann 3 vuotta sitten
213
Lisää tämän kaltaisia
Goal continued, medicated during my shift with 40meq potassium po and 10meq IV. Brought level up to 3.2.
Teaching #2 - Teach patient to read nutrition labes
rationale - teach the patient to take charge of their nutrion
Teaching #1 - teach patient which foods are high in potassium leafy greens, nuts, etc. - teach patient about low sodium - salt substitutes
rationale - regulate labs, prevent dysrhythmias, lead a healthy life
Collaborative Intervention #2 - work with patient and family to implement a heart healthy, kidney healthy diet.
Collaborative Intervention #1 - work with dietary to provide a low sodium, high potassium, cardiac diet
Rationale - keep potassium and sodium levels under control
Teaching #2 - Teach patient about medication resources
Teaching #1 - teach patient organization for medication times, make a calendar/schedule
rationale - medication adherence
Collaborative Intervention #2 - work with patient and family for at home medication adherence
Collaborative Intervention #1 - work with doctor and pharmacy to provide potassium supplementation.
Rationale - monitoring lab work will tell the nurse what interventions need to be done to fix the specific lab levels
systolic blood pressure over 100 the entirety of my shift, this is a continued goal.
Teaching #2 - safety when ambulating - non slip socks, utilize any assistive devices, walk with someone not alone
Rationale - to prevent falls
Teaching #1 - benefits of movement
rationale - to prevent atelectasis and work the edema out of the interstitial spaces.
Collaborative Intervention #2 - encourage patient to utilize deep breathing / incentive spirometer alone, with family or staff help
Collaborative Intervention #1 - encourage the patient to work with PT/OT, techs, students, or other nurses to ambulate as much as possible
Rationale - CHF patients are at risk for atelectasis when they are in the hospital due to being sedentary
Teaching #2 - Do not dump urine with out measuring
Rationale - We need to measure all urine to be able to identify and prevent fluid volume overload
Teaching #1 - How to urinate in the hat
Rationale - We need to collect the urine in a hat for measurement
Collaborative Intervention #2 - work with other nurses, techs, students, family to measure all oral intake for the patient - report all oral intake to the nurse for charting
Collaborative Intervention #1 - work with other nurses, techs, students, family to measure urine output for the patient - report all output to the nurse for charting
Rationale - avoid fluid volume overload - do not make a sick heart work harder